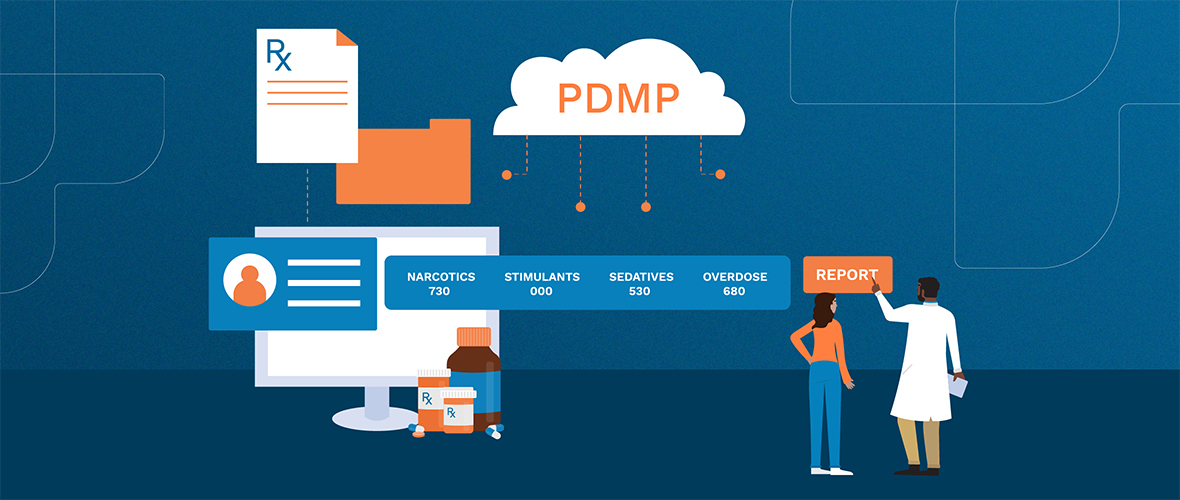
Does your state have a Prescription Drug Monitoring Program (PDMP)? A PDMP (aka PMP) is a state-based database of controlled substances dispensed to patients from different providers. They aren’t new—in fact, they’ve existed for more than 100 years. But PDMP technology advancements have made it easier for doctors and pharmacists to track certain prescription drugs to prevent abuse and misuse.
However, there are no standard requirements and each state manages their PDMP differently. Especially when it comes to integrating with healthcare technology, such as Electronic Health Records (EHR) and E-Prescribing (eRx).
Diverse ways of funding
PDMP financing comes from many different sources, including private and public grants, licensing fees, donations, registration fees, surcharges, insurance fees, and general revenue. Some states require fees from drug manufacturers, but some prohibit fees as a way to fund PDMPs.
And the Centers for Medicare and Medicaid Services (CMS) authorize 100% federal funding support to states to help pay for technology that addresses the opioid crisis among Medicaid beneficiaries.
No matter who pays for PDMP implementation and maintenance, not all states provide funding to connect with EHRs and eRx software. Instead, in certain states, providers foot the bill.
Why integration funding is important
As you would expect, there are many advantages to direct PDMP access from your healthcare software:
- More interoperability and integration with EHR and eRx systems
- Greater information sharing between providers, physician offices, and pharmacists
- Ability to exchange data between prescribers in border states and across state lines
- Data transparency and other features to better deliver actionable predictive information
Research suggests that PDMPs with funded integration generate better health outcomes. The Centers for Disease Control and Prevention (CDC) reviewed PDMPs during the period between 2010 and 2015. In one example, Ohio’s funded PDMP showed a decrease of opioid prescriptions in 85% of their counties, while neighboring state Kentucky, which doesn’t have a fully-funded PDMP, showed a decrease in 62% of its counties.
Is your state’s PDMP integration funded?
As of May 2021, PDMPs are available in all 50 states, D.C., and Guam, with less than half being fully funded. Missouri was the last state to implement a statewide PDMP after the State Legislature gave final approval with the SB 63 bill.
Funding and integration status changes frequently. Check here for updates.
PDMPs required in most states
Even in those cases where PDMP integration is not fully funded, data from the CDC shows that they can be effective. And no matter the funding status, you must use a PDMP when prescribing certain substances unless you practice in one of these states: Kansas, Idaho, Missouri, Montana, Nebraska, Oregon, South Dakota, and Wyoming. If you’re not already registered with your state’s PDMP, contact your state for more information.
RXNT offers direct access to state PDMPs through Bamboo Health (formerly Appriss Health). It’s conveniently integrated into RXNT’s Electronic Health Records (EHR), Electronic Prescribing (eRx), and Full Suite solutions—so there’s no interruption to a provider’s workflow.