About 63% of denied claims are potentially recoverable through appeals. However, that’s only possible if practices have the right systems and processes in place.
Healthcare practices across the United States are facing an escalating challenge that directly impacts their financial stability: denials. With initial denial rates reaching 11.8% in 2024, up from 10.2% in 2020, healthcare providers are losing substantial revenue to claim rejections. The stark reality is that U.S. hospitals lose an estimated $262 billion annually due to initial claim denials, meaning that effective denial management in medical billing is not just important, it’s essential not only for practice growth but survival.
The good news? About 63% of denied claims are potentially recoverable through appeals. However, that’s only possible if practices have the right systems and processes in place! That’s why understanding denial management is critical for every healthcare organization.
Understanding Denial Management in Healthcare
Denial management is a strategic process focused on identifying, reviewing, and resolving claim denials to ensure healthcare providers receive appropriate reimbursement for services rendered. It represents a critical component of revenue cycle management that directly impacts a healthcare organization’s financial stability.
At its core, effective denial management for medical billing requires a systematic approach to identifying and resolving claim rejections. This process demands more than simply resubmitting denied claims—it requires understanding why denials occur, implementing prevention strategies, and developing efficient resolution workflows.
The financial implications are substantial. Healthcare providers spend approximately $19.7 billion annually on appeals of denied claims, with each denied claim costing between $25 and $181 to correct and resubmit. When approximately 15% of submitted charges are denied by payers, the cost of denied claims and especially unappealed denials can compound quickly.
Modern denial management for healthcare organizations typically leverages technology to streamline the appeals process and improve recovery rates. However, the foundation of successful medical billing denial management lies in understanding common denial patterns and implementing both preventive measures and efficient resolution strategies.
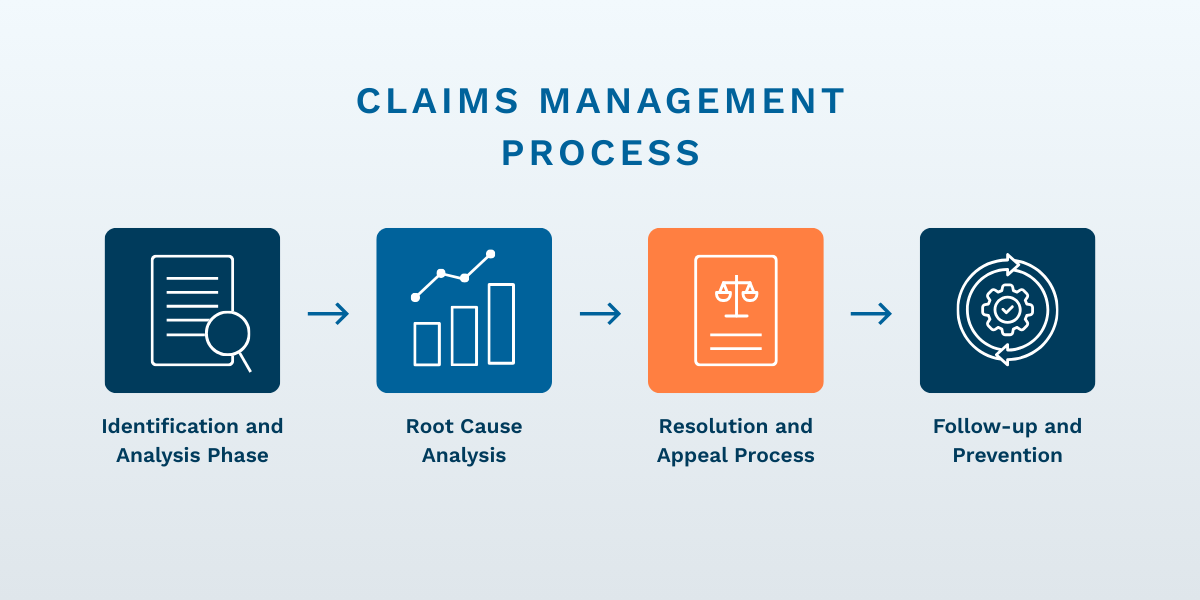
The Claims Denial Management Process
The denial management process in medical billing involves identifying, analyzing, and resolving rejected claims through a structured workflow. Understanding this process is crucial for healthcare practices trying to improve their revenue recovery rates.
Identification and Analysis Phase
The first step of denial management for healthcare organizations and medical billing teams is to systematically track and categorize denials. Healthcare practices must distinguish between “hard denials” (non-recoverable claims that are permanently rejected) and “soft denials” (temporary rejections that require additional information but may be recoverable with proper follow-up).
Effective claims denial management can recover up to 63% of initially denied claims, but this requires immediate identification and proper categorization. Practice Management and Medical Billing software systems play a crucial role here by automatically flagging denied claims and categorizing them based on denial codes and reasons.
Root Cause Analysis
Successful claims management requires identifying root causes and implementing corrective measures. This involves analyzing denial patterns to determine whether issues arise from front-end processes (such as insurance verification), coding errors, or documentation issues. Data verification and validation become essential components of this analysis phase.
Resolution and Appeal Process
The resolution phase involves preparing and submitting appeals, gathering necessary documentation, and maintaining communication with payers. This is where streamlining the denial management process in medical billing can significantly improve practice profitability. Automated workflow management reduces manual errors and accelerates processing times.
Follow-up and Prevention
It’s essential to ensure prevention, and the final phase focuses on implementing changes to prevent similar denials in the future. This includes updating front-end verification processes, improving staff training, and enhancing documentation practices.
Common Causes of Medical Billing Denials
Understanding the common reasons behind medical billing denials helps practices develop better prevention strategies. Recent data reveals that 50% of denials stem from missing or inaccurate data, while 35% are due to authorization issues.
Missing or Incorrect Information
The most common cause of denials is missing or blank fields, incorrect patient details, or inaccurate insurance information. These administrative errors are entirely preventable with proper front-end verification processes and real-time eligibility checking.
Authorization Issues
Missing prior authorization, expired authorizations, or services outside the approved scope represent significant denial categories. A properly trained team and practice management technology can help by maintaining authorization databases and providing alerts when authorizations are approaching expiration.
Medical Necessity and Documentation
Insufficient documentation, services deemed unnecessary, and a lack of supporting evidence account for a substantial portion of denials. These issues often require enhanced communication between clinical and billing staff.
Coding and Billing Errors
Incorrect codes, bundling issues, and duplicate submissions continue to plague healthcare practices. Advanced, modern medical billing systems can help prevent these errors through automated code validation and duplicate checking.
The Role of Practice Management and Medical Billing Software
Practice Management software has become indispensable for effective denial management, offering automated solutions that address the most common causes of claim rejections. Modern systems can achieve a 98% first-pass clean claims rate when properly implemented and utilized.
Automated Claim Verification
Practice Management systems provide real-time error detection before claims submission, catching issues like missing information, incorrect codes, or eligibility problems. This front-end verification prevents many denials from occurring in the first place.
Integrated Workflow Management
These systems integrate scheduling, billing, and patient management functions, ensuring data consistency across all touchpoints. When patient information is entered once and shared across all modules, the risk of data entry errors decreases significantly.
Analytics and Reporting Capabilities
Medical billing and revenue cycle management platforms offer root-cause analysis and reporting tools, trend identification features, and performance tracking capabilities. Real-time, advanced reporting helps practices identify denial patterns and implement corrective measures quickly.
Electronic Health Records Integration
Seamless data sharing between Practice Management systems and Electronic Health Records improves documentation accuracy and enhances coding precision. This integration ensures clinical note-taking and encounters meet billing requirements at the point of care.
The impact of technology on denial management cannot be overstated. Practices using integrated Practice Management software alongside a trained, professional billing team report reduced manual errors, faster processing times, and improved overall efficiency in their denial management workflows.
In-House vs. Outsourced Denial Management
Many healthcare practices face a critical decision when developing their denial management strategy: manage denials internally with a billing team or outsource billing work to a specialized company. Each approach offers distinct advantages and challenges that practices must carefully evaluate.
In-House Management Advantages
Practices that opt for internal denial management with a billing department often want direct control. With this option, the practice maintains immediate access to billing information, can respond quickly to issues, and enhances patient relationship management through personalized attention. Team integration improves communication between clinical and billing staff, streamlining workflows and enabling more efficient denials resolution.
However, in-house management can be resource-intensive, resulting in higher operational costs, dedicated staffing, and ongoing training requirements. Some practices struggle with limited expertise, finding it difficult to keep up with constantly changing regulations and payer requirements.
Outsourced Management Benefits
Outsourcing denial management—or even the entire revenue cycle—to a trusted billing and RCM partner provides access to specialized expertise, up-to-date regulatory compliance guidance, and advanced technology solutions that many practices cannot afford to implement independently. Cost efficiency is evident through reduced overhead, elimination of training costs, and scalable solutions that adapt to practice volume.
The primary disadvantage of this option involves less control over the process. Practices may experience less direct oversight, communication challenges, and potential misalignment of priorities between the practice and the vendor.
Making the Right Choice
The decision between in-house vs. outsourced denial management depends on practice size, available resources, and internal expertise. Smaller practices often benefit from outsourcing, while larger organizations may prefer maintaining internal control. Some practices adopt hybrid approaches, managing certain types of denials internally while outsourcing complex appeals.
Key Considerations When Evaluating Denial Management Software or Solutions
Healthcare practices implementing robust denial management in medical billing see significant improvements in revenue recovery, but success requires careful evaluation of several key factors.
Technology Integration
Practices must assess how well potential solutions integrate with existing systems. Seamless integration between Practice Management software, Electronic Health Records, and billing systems ensures data consistency and reduces manual data entry errors.
Staff Training on Technology
Successful implementation requires comprehensive staff training strategies. Practices should evaluate the learning curve associated with new systems and plan for adequate training time and resources.
Metrics and Reporting
Effective denial management requires robust analytics capabilities. Practices should prioritize solutions that offer detailed reporting on denial trends, resolution rates, and financial impact. Key performance indicators should include first-pass clean claim rates, denial resolution timeframes, and recovery percentages.
Scalability and Growth
Solutions should accommodate practice growth and changing needs. Practices should evaluate whether systems can handle increased volume and additional locations without significant additional investment.
Compliance and Security
Given the sensitive nature of healthcare data, practices must ensure that whichever denial management solution is chosen meets all regulatory requirements and provides appropriate security measures.
Best Practices for Effective Denial Management
Healthcare providers lose billions annually due to unresolved medical billing denials, but implementing best practices can significantly improve recovery rates and prevent future denials.
- Prevention-Focused Approach – The most effective denial management strategy emphasizes prevention over resolution. This includes implementing robust front-end verification processes, maintaining current insurance eligibility databases, and ensuring proper authorization management.
- Education and Training – Regular training on coding updates, payer requirements, and documentation standards helps prevent denials at the source. Cross-training staff members ensures continuity in denial management processes.
- Technology Utilization – Leveraging Practice Management technology for automated verification, real-time error detection, and workflow management significantly improves denial management efficiency.
- Performance Monitoring – Regular monitoring of denial rates, resolution timeframes, and recovery percentages helps practices identify areas for improvement and measure the effectiveness of their denial management strategies.
Moving Forward with Confidence
Effective denial management in medical billing represents both a challenge and an opportunity for healthcare practices. While denial rates continue to rise, practices that implement systematic approaches to denial prevention and resolution can recover substantial revenue and improve their financial stability.
The key lies in understanding that denial management is not just about appealing rejected claims—it’s about creating systems and processes that prevent denials from occurring and efficiently resolve those that do. Practice Management software plays a crucial role in this process, offering automated solutions that address the most common causes of denials.
Whether practices choose in-house management, outsourcing, or a hybrid approach, success depends on having the right systems, trained staff, and a commitment to continuous improvement. By focusing on prevention, leveraging technology, and maintaining vigilant monitoring of performance metrics, you can transform denial management into a revenue recovery engine. For healthcare practices serious about their financial health, developing a robust denial management strategy is not optional—it’s essential for long-term success.