The ABCs of SOAP Notes for Practices
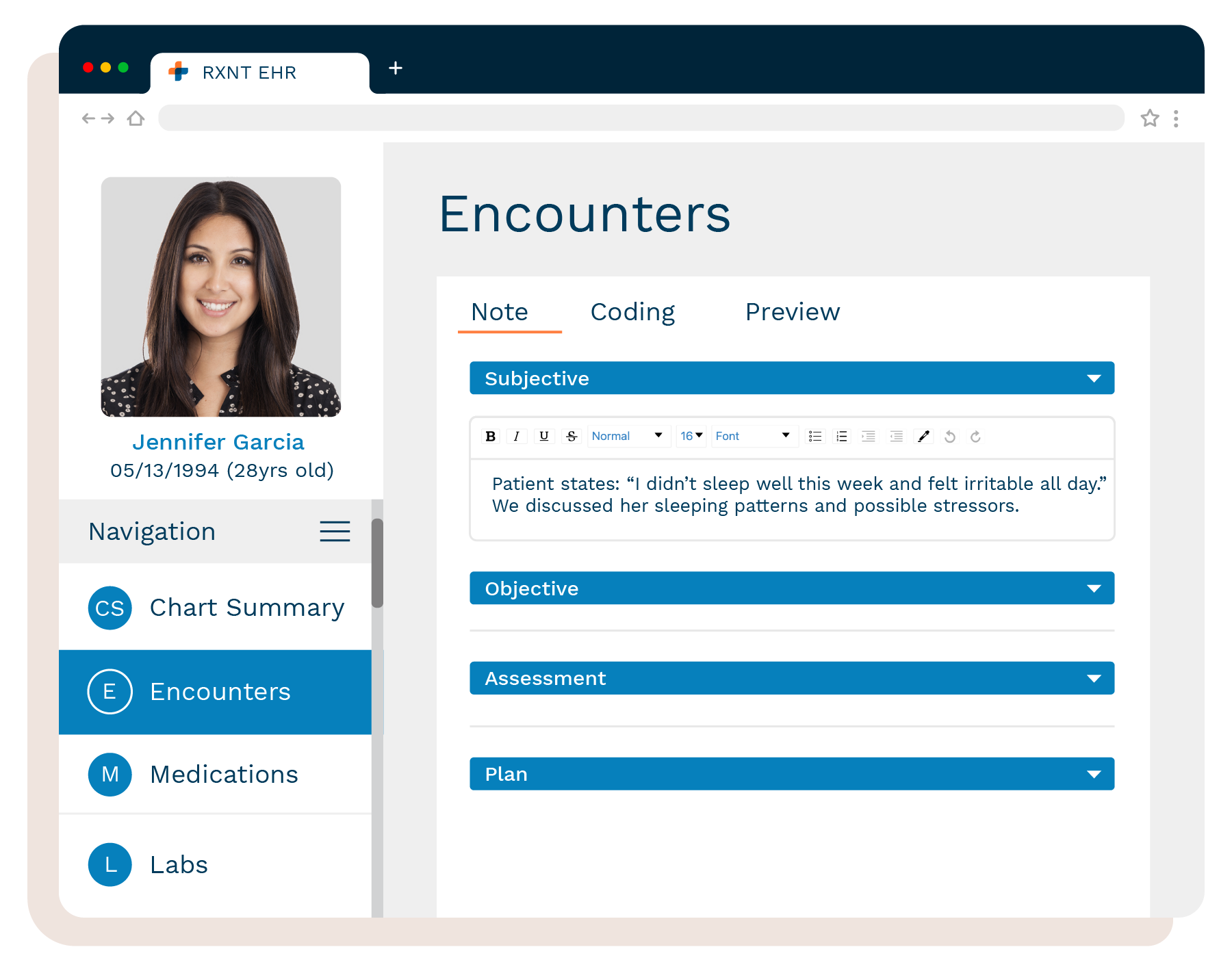
The acronym SOAP stands for Subjective, Objective, Assessment, and Plan. This standardized method of documenting patient encounters allows providers to concisely record patient information. The notetaking method also makes it easier to share patient information between healthcare professionals, minimizing confusion and misinterpretation.
Subjective
This first component details the patient’s complaint or what brings them to the healthcare provider’s office. It includes their symptoms, when those symptoms started, the frequency and severity of the symptoms, the region of the body affected, and other relevant information such as family history, social history, as well as past and present illnesses.
Objective
Next, you’ll record measurable and quantifiable information. This information includes the patient’s vital signs, notes from the doctor’s physical exam, allergies, and reports from diagnostic tests (e.g., blood tests and imaging).
Assessment
For assessment, you’ll document the physician’s analysis. It should include diagnoses, patient progress, and evaluation of medication or treatment. Although it’s a summary statement, it should not repeat information in the Subjective and Objective sections.
Plan
Finally, the fourth section records the patient’s treatment plan for their condition, such as medications, additional procedures and diagnostic tests (if needed), referrals, goals, and follow-up steps. In the case of a previous treatment plan, you don’t need to rewrite the information, but it’s critical to include changes to an existing plan.
The ABC's of SOAP Notes for Practices
The acronym SOAP stands for Subjective, Objective, Assessment, and Plan. This standardized method of documenting patient encounters allows providers to concisely record patient information. The notetaking method also makes it easier to share patient information between healthcare professionals, minimizing confusion and misinterpretation.
Subjective
This first component details the patient’s complaint or what brings them to the healthcare provider’s office. It includes their symptoms, when those symptoms started, the frequency and severity of the symptoms, the region of the body affected, and other relevant information such as family history, social history, as well as past and present illnesses.
Objective
Next, you’ll record measurable and quantifiable information. This information includes the patient’s vital signs, notes from the doctor’s physical exam, allergies, and reports from diagnostic tests (e.g., blood tests and imaging).
Assessment
For assessment, you’ll document the physician’s analysis. It should include diagnoses, patient progress, and evaluation of medication or treatment. Although it’s a summary statement, it should not repeat information in the Subjective and Objective sections.
Plan
Finally, the fourth section records the patient’s treatment plan for their condition, such as medications, additional procedures and diagnostic tests (if needed), referrals, goals, and follow-up steps. In the case of a previous treatment plan, you don’t need to rewrite the information, but it’s critical to include changes to an existing plan.
-
Interoperability & Productivity
With the SOAP note format, healthcare providers benefit from enhanced communication and ensure higher standards of patient care through consistent documentation.
-
Better Patient Outcomes
Practitioners can better diagnose patients, formulate treatment plans to meet the desired outcomes, and track progress toward those goals.
-
Drive Efficiency & Simplicity
Clinicians can simplify charting and better organize information by capturing patient data through a standardized, predictable, understandable template.
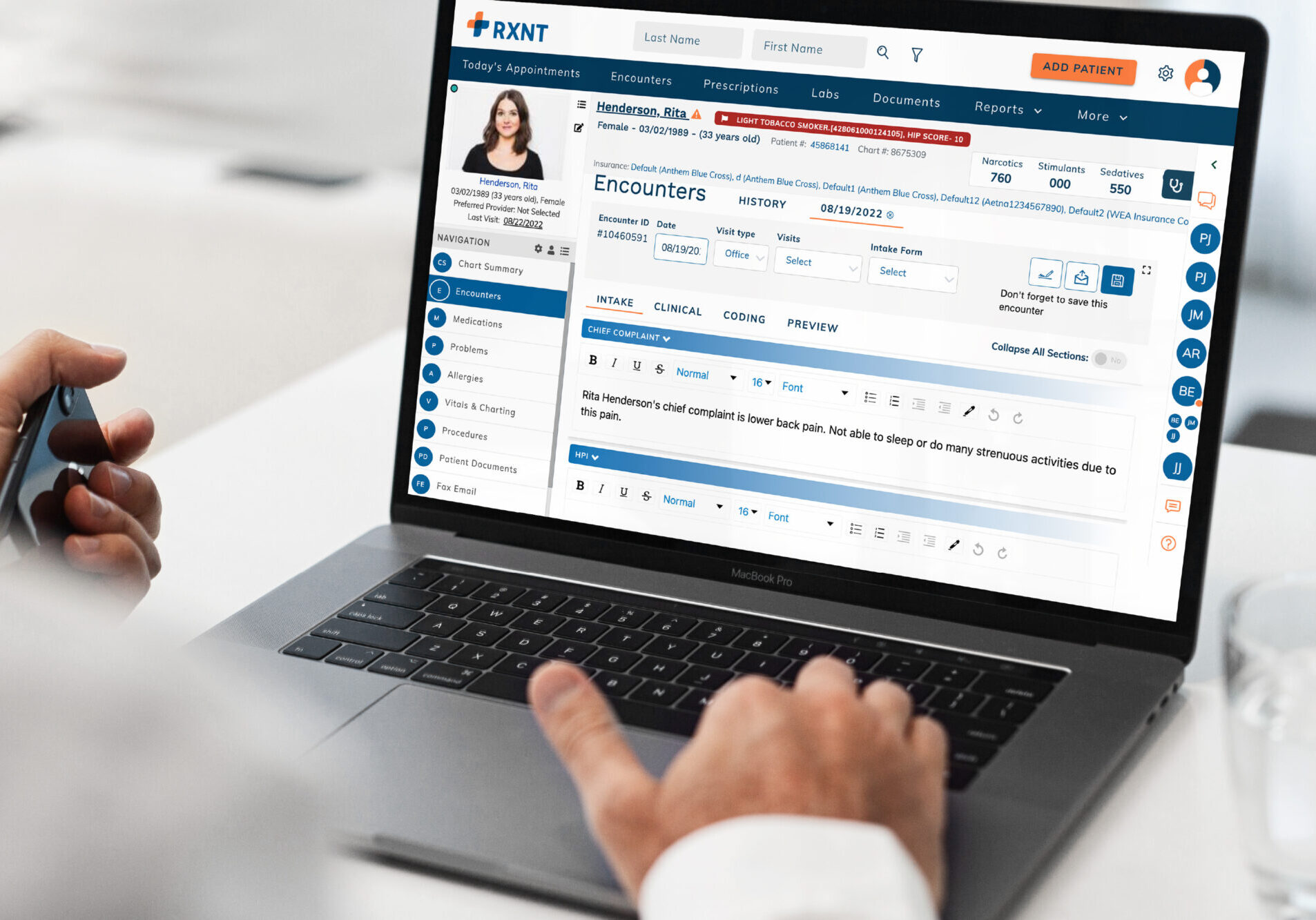
SOAP Notes + Electronic Health Records (EHR) = Better Communication
As interoperability expands throughout the healthcare industry, best practices such as SOAP notes simplify the sharing of patient information across EHR systems and providers. Consistent documentation improves provider-to-provider communication, reduces redundant tests and imaging, and enhances health outcomes.


Minimize Record Errors and Ensure Patient Safety
Consistent documentation protects patients while reducing the risk of medical errors and malpractice claims. SOAP notes can help minimize medical record errors and communication failures that have resulted in 37% of high-severity injury cases, according to a 2016 study.
Interested in learning more about reducing practice risk? Check out RXNT’s Risk Awareness toolkit packed with resources to help practitioners identify risks and proactively address them.
Reduce Provider Burnout
In 2021, the burnout rate for physicians reached an all-time high of 62.8%, according to a Mayo Clinic study from September 2022. With additional strains on the healthcare system and increased public health demands, providers need a simplified, standardized way to capture critical information. Writing SOAP notes provides a simplified cognitive framework and reduces the note-taking burden for clinicians, allowing for more time for patients.
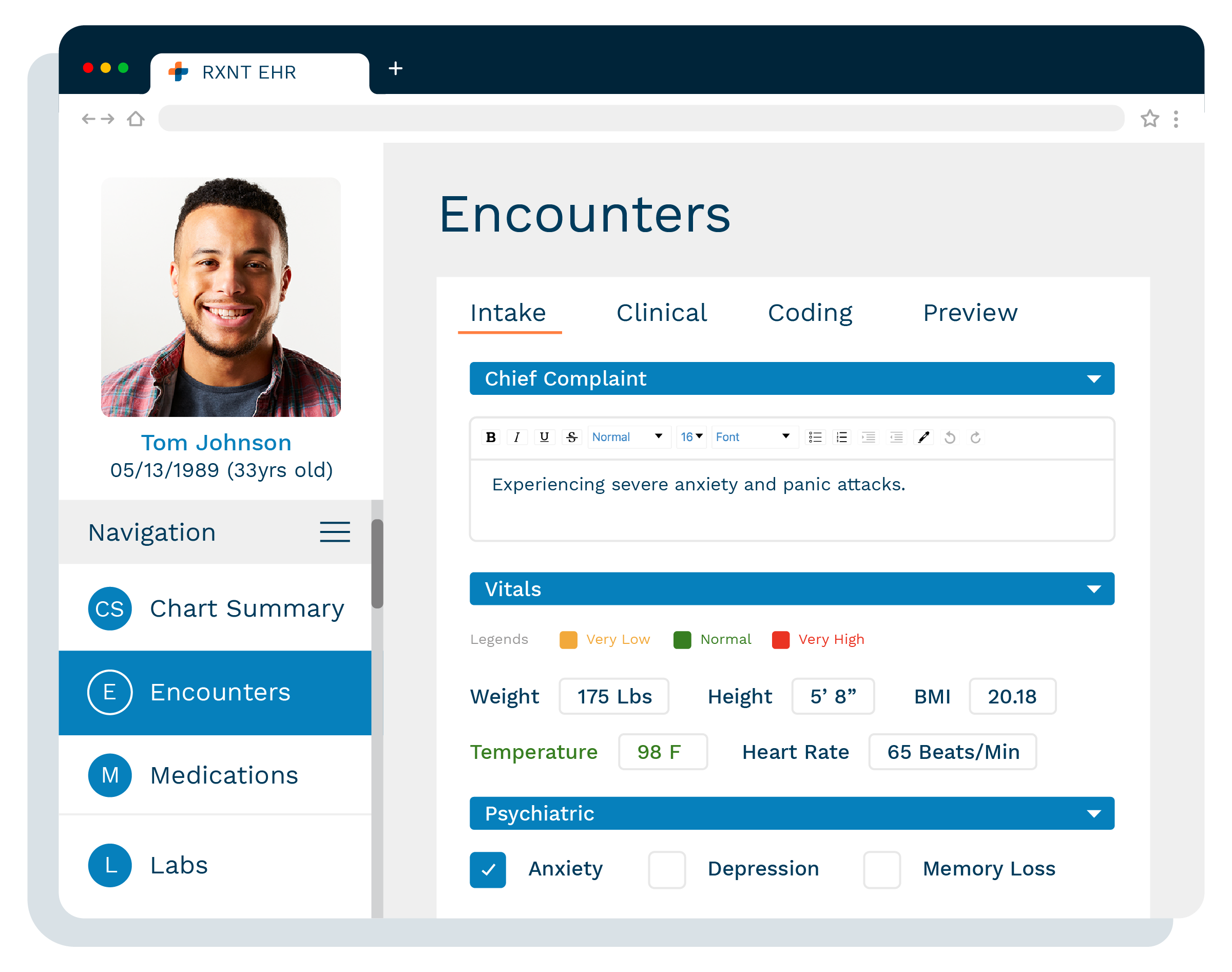
Customizable Smart Forms for SOAP Notes
RXNT offers custom Smart Forms for EHRs to help you tailor encounters and documentation to your practice. Hundreds of forms are available, including a Basic and a Detailed SOAP form with separate “plug-ins” for Vitals, Allergies, Medications, and Orders. Save time and reduce clicks with Short Keys and Procedure Macros. With these functions, you can quickly add commonly-used text blocks to your encounter templates.
"Very intuitive. Easy to navigate. Much more user friendly than competing programs."
Gabrielle
"There are such a significant number of advantages, I don't know where to begin! The staff at RXNT is awesome."
Federico
"Great value, integrated system. Have used daily for years and keeps getting better"
Mike
See our SOAP note template in action!
Get an easy, virtual demo to learn more about SOAP notes or to see how RXNT's other customizable templates will help create efficiencies and streamline your practice. Our friendly, no-pressure customer advisors will answer any questions and help you to evaluate your needs.
Used in healthcare organizations of all sizes, from small family clinics to large, multi-specialty practices—we offer flexible pricing options to make our tools accessible to almost any practice. Every product is backed by 24/7 cloud-based access, premium in-house support, and regular system upgrades.