Understanding the Merit-Based Incentive Payment System (MIPS)
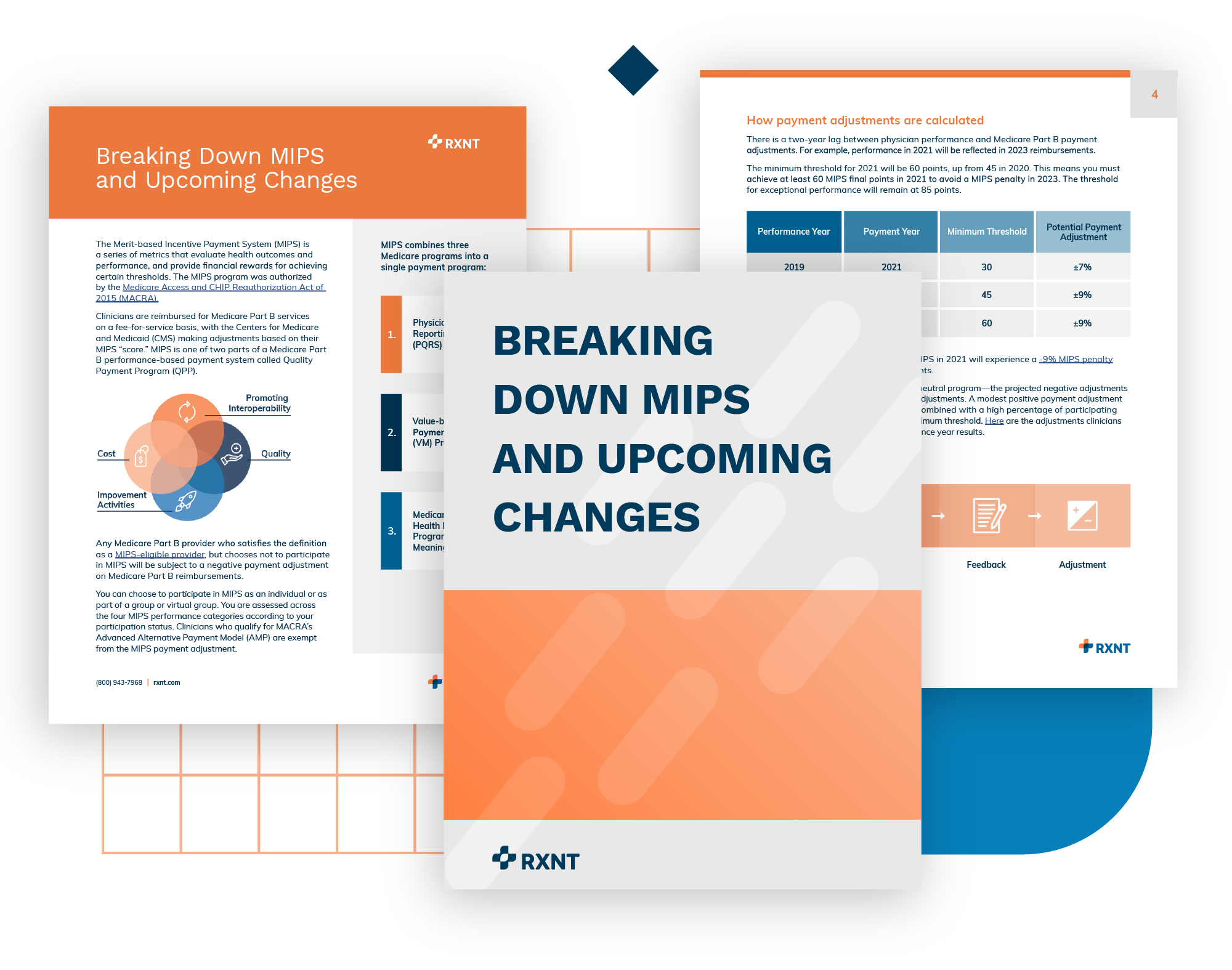
The Merit-based Incentive Payment System (MIPS) is a series of metrics that evaluate health outcomes and performance, and provide financial rewards for achieving certain thresholds. The MIPS program was authorized by the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA).
Clinicians are reimbursed for Medicare Part B services on a fee-for-service basis, with the Centers for Medicare and Medicaid (CMS) making adjustments based on their MIPS “score.” MIPS is one of two parts of a Medicare Part B performance-based payment system called Quality Payment Program (QPP).
What's covered in this guide?
-
MIPS eligibility at-a-glance
Determine if you qualify as a MIPS-eligible provider.
-
Performance measurements & incentives
Categories are weighted, with metrics defining financial incentives.
-
What's new for MIPS in 2021?
These significant changes are taking effect in 2021.
Get the full white paper
We build software for physicians and healthcare professionals. If you are a patient, please contact your doctor. If you are having a medical emergency or need urgent help, call 911.
White Paper Download
"*" indicates required fields
MIPS Value Pathways (MVPs) are the newest MIPS reporting option (an alternative to "traditional MIPS" and "APM Performance Pathway") that you can use to meet your MIPS reporting requirements.
Source: qpp.cms.gov